Front of Card
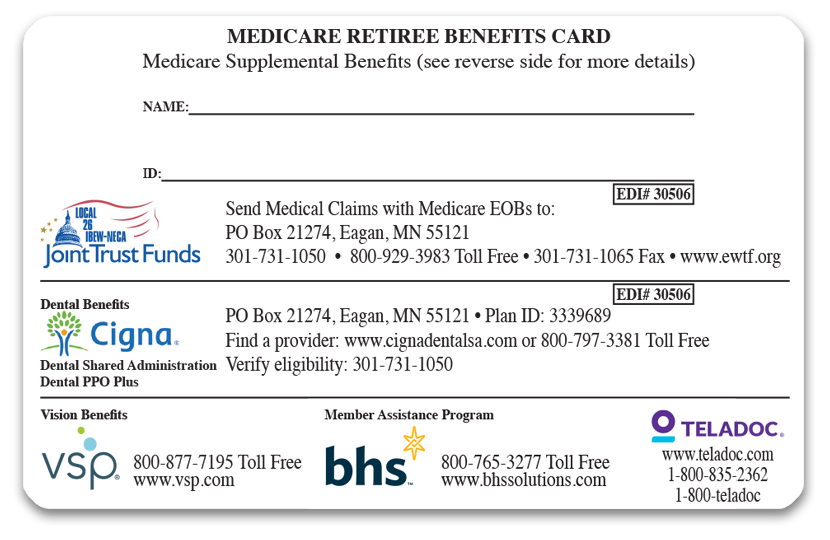
MEDICARE RETIREE BENEFITS CARD
This is your Medicare Supplemental ID Card.
Medicare Supplemental Benefits
Provides additional information for members and providers
NAME:
Member/Dependent full name Including middle initial
ID:
This is the member’s 6 digit alternate ID# which is used for both members and Medicare primary dependents (spouses and disabled dependents)
JOINT TRUST FUNDS:
Address for providers or members to send Medicare claims with EOB’s – phone and web contact information
CIGNA:
Provider address information for submitting dental claims
Dental Shared Administration
Name of dental services
Dental PPO Plus
Type of dental plan for members to locate participating providers
Find a Provider:
Web address and phone number for members to locate participating providers
Verify Eligibility:
Provider’s contact phone number for verifying dental benefits
VSP
Phone number and web address for members to confirm eligibility and locate a participating provider
BHS
Contact information phone and web Address for mental health and chemical dependency help
TELADOC
Web address and phone contact information for virtual physicians 24/7 access phone or video
Back of Card
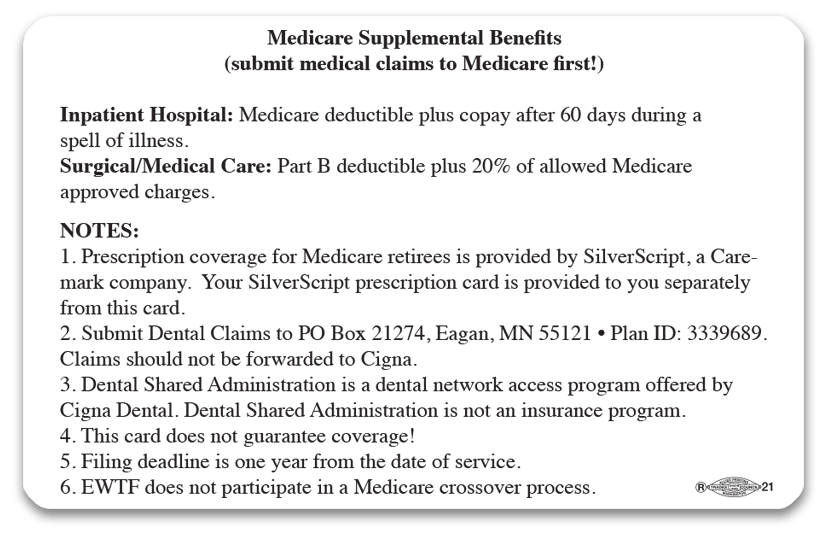
Medicare Supplemental Benefits
Notification that EWTF is your secondary insurance and will supplement Medicare coverage
Inpatient Hospital:
EWTF will pay Medicare deductible plus co-pay after 60 days during a spell of illness
Surgical/Medical Care:
EWTF will pay your Part B deductible plus 20% of allowed Medicare approved charges
Prescription Coverage
Provided by Caremark through SilverScript--Members should have a SilverScript prescription card in addition to your Medicare Supplemental card
Submit Dental Claims
Providers to submit claims to address provided and use Plan ID #
Dental Shared Administration
Your dental network access and not an insurance program
This Card Does Not Guarantee Coverage!
Medical providers should verify your eligibility--do not use this card if you are not eligible for benefits through EWTF
Filing Deadline is One Year From the Date of Service
You or your provider should submit your claims to EWTF by no later than one year from the date of service (timely filing date). If not, claims will be denied
EWTF Does Not Participate in a Medicare Crossover Process
EWTF does not transfer processed claim data to Medicaid, state agencies, or other insurance programs
